Every evening, when it was time to return home to their eight other children, parents Katie and Dan steeled themselves to say goodnight to their youngest. Their newborn son, Joseph, had been born with multiple heart defects, and was now in Connecticut Children’s pediatric cardiovascular intensive care unit (PCVICU) — a special unit for patients with severe heart conditions.
For Katie and Dan, this was a new and heart wrenching experience: “I’ve had a lot of babies. I’m not used to having other people take care of them,” Katie says.
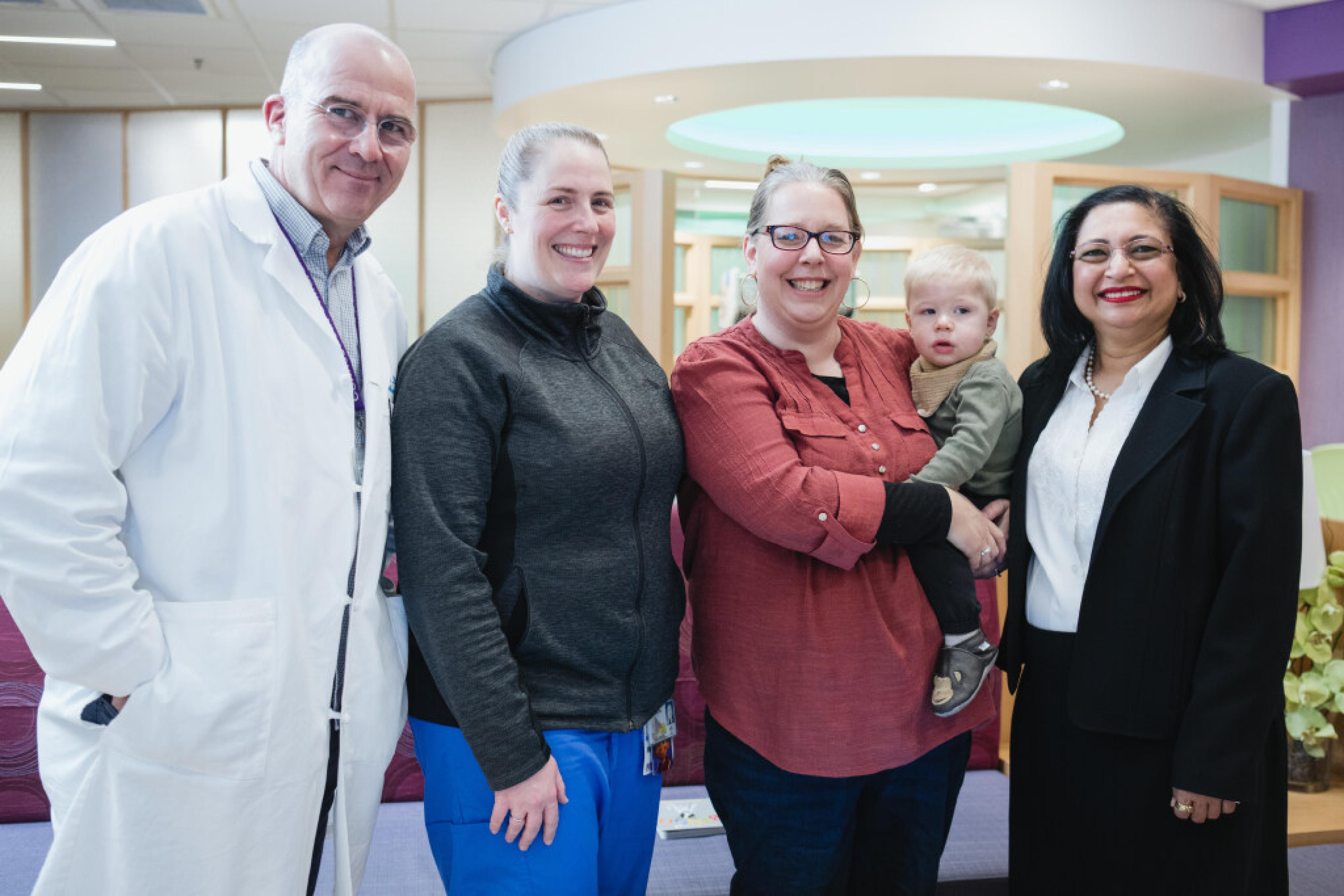
But ultimately, it was that same team, led by pediatric cardiac intensivist Monika Gupta, MD, who gave them the confidence to step away.
“We knew the cardiac ICU team loved Joseph too,” says Katie.
“We consider ourselves as not just medical providers, but as a part of our patient's larger family,” says Dr. Gupta.